May 4, 2023
Submitting a corrected claim may be necessary when the original claim was submitted with incomplete information (e.g., procedure code, date of service, diagnosis code). The preferred process for submitting corrected claims is to use the 837 transaction
for both professional and facility claims, and claim frequency code 7.
To submit a corrected paper claim:
- Submit as a replacement claim, clearly marking the claim as a corrected claim; failure to indicate that a claim is a corrected claim may result in a denial as a duplicate claim.
- Bill all original lines - not doing this will cause the claim to be rejected.
- Attach a completed Corrected Claim - Standard Cover Sheet.
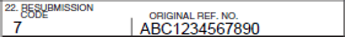
- In box 22 on the CMS-1500 Claim form, enter the appropriate bill frequency code, left justified in the left hand side of the field. Use the following codes:
- 7–Replacement of prior claim
- 8–Void/cancel of prior claim
- In the Original.Ref.Co segment of box 22 enter the original claim number
EXAMPLE:
Standard Cover Sheets are available under Forms on our provider website.
To submit a corrected claim electronically:
Use the HIPAA 837 standard claims transaction include the following information:
- Frequency code of “7” in loop 2300, CLM05-3 segment to indicate a corrected/replacement of a previously processed claim. Use “8” to void a claim billed in error.
- The initial claim number (in loop 2300, REF01 must contain “F8” and REF02 must contain the claim number)
- A free form note with an explanation for the corrected/replacement claim, in loop 2300 claim note as:
- For professional and dental claims: segment NTE01 must contain “ADD” and segment NET02 must contain the note, for example: NTE*ADD*CORRECTED PROCEDURE CODE (or the data element was corrected/changed on the claim)
- For facility/institutional claims: segment NTE01 must contain “UPI” and segment NTE02 must contain the note, for example: NTE*UPI*CORRECTED LAB CHARGES (or the data element was corrected/changed on the claim)