July 7, 2022
When
using Availity to check dental benefits, remember to choose “Premera Dental” as
the payer:

You
can find a patient’s dental claim history by clicking on the blue Services
History button at the top of the member’s eligibility and benefits page. This
button displays only when you select Premera Dental as a payer.

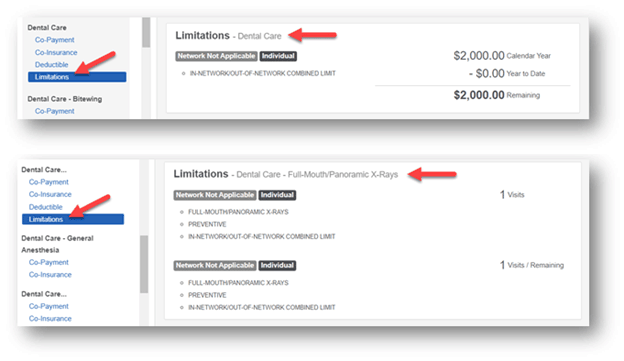
Verify
benefit limits
If you’re looking for a
member’s dental services benefit limits, you can:
- Scroll through
the list of benefits to find the specific service limitations
- Use control F
to open a search box and use the keyword ‘limit’ to view all dental services
that have limitations.
If you need a dental fee schedule and are contracted with United Concordia (and not Premera), contact United Concordia directly.
Sign up for
training webinars
Several training webinars are now available, including Premera-specific training. All webinars are in Pacific Time.
Availity Introduction for Premera
Providers
August 9, noon to 1 pm
August 23, 11 am to noon
Dental Claim Submission and Claims
Follow-up for Premera Providers
August 16, noon to 1:30 pm
August 30, 11:30 am to 1 pm
Register and Get Started with Availity
July 12, noon to 12:30 pm
August 9, 10 to 10:30 am
Resources and Tips for New Administrators
July 27, noon to 1 pm
August 24, 10 to 11 am
To register, sign in to Availity,
select Help & Training > Get Trained and then select Sessions in the
Search Catalog field. To see all the trainings listed for the current month,
you can scroll the list. If you want to view sessions for a specific day,
select that day on the calendar under Your Calendar. For recorded
trainings, enter "PREMERA" in the Search Catalog field, and
then select the course you want.
If you have questions about Availity, visit availity.com/premera.
For more Premera dental provider information, visit our Dental Resources page.